v
Care Transitions InterventionSM
v
With funding from The John A. Hartford Foundation
and The Robert Wood Johnson Foundation, the
Care Transitions InterventionSM was designed in response to the need for a patient-centered,
interdisciplinary intervention that addresses continuity of care across multiple settings and
practitioners. The overriding goal of the intervention is to improve care transitions by providing
patients with tools and support that promote knowledge and self-management of their condition as they
move from hospital to home.
The model is composed of the following components:
- A patient-centered record that consists of the essential
care elements for facilitating
productive interdisciplinary communication during the care transition (referred to as the
Personal
Health Record, or PHR).
- A structured checklist (Discharge Preparation
Checklist) of critical activities
designed to empower patients before discharge from the hospital or nursing facility.
- A patient self-activation and management session with a Transition Coach (Geriatric Nurse
Practitioner) in the hospital-designed to help patients and their caregivers understand and apply
the first two elements and assert their role in managing transitions.
- Transition Coach follow-up visits in the Skilled Nursing Facility (SNF) and/or in the home and accompanying phone calls designed to sustain the first three components and provide continuity across the transition.
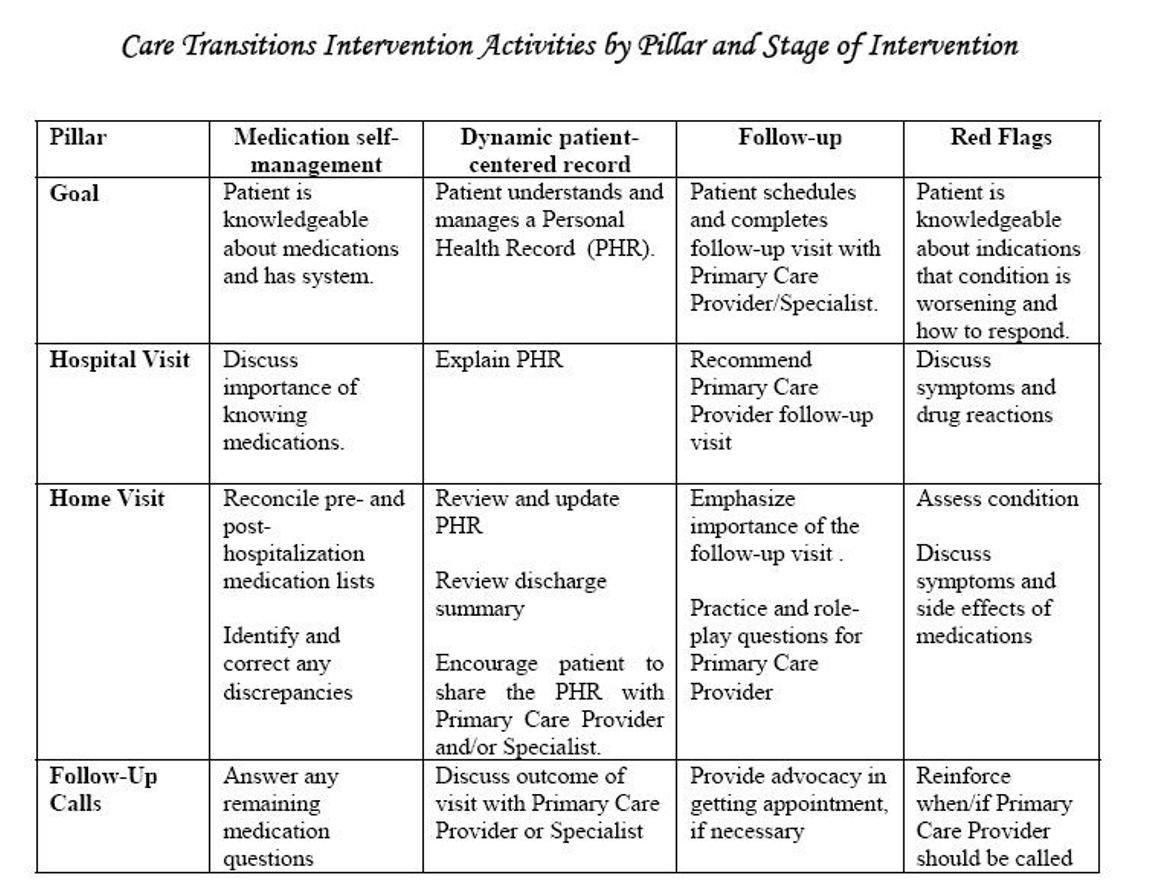
The intervention focuses on four conceptual areas, referred to as pillars:
- Medication self-management: Patient is knowledgeable about medications and has a medication management system.
- Use of a dynamic patient-centered record: Patient understands and utilizes the Personal Health Record (PHR)
to facilitate communication and ensure continuity of care plan across providers and settings. The patient or informal caregiver manages the PHR.
- Primary Care and Specialist Follow-Up: Patient schedules and completes follow-up visit with the primary care physician or specialist physician
and is empowered to be an active participant in these interactions.
- Knowledge of Red Flags: Patient is knowledgeable about indications that their condition is worsening and how to respond.
 |
The intervention design is outlined in detail in two venues:
a Protocol Manual
and the publication: “The Care Transitions Intervention: A Patient-Centered
Approach to Facilitating Effective Transfers Between Sites of Geriatric Care”, Home Health Services
Quarterly, 2003;22(3):1-18.
Findings:
Abstract of article: Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: The care transitions intervention. J Am Geriatr Soc. 2004;52:1817-1825.
v
 |
v
